Latest News
March 22, 2011
By DE Editors
The medical establishment already has a very clear picture of cataracts and how to treat them. That’s encouraging, given the fact that by age 80, more than 50 percent of all Americans will have developed a cataract—and every year, more than 3 million will undergo eye surgery to correct it. What is also encouraging is the surgical outcome: the success rate is 95 percent, with vision typically restored within a 20/20 (normal) to 20/40 (good) range.
|
Modern cataract surgery was first performed in the late 1960s, enabled by the development of an ultrasound technology that emulsified the eye’s diseased natural lens, along with the discovery of a suitable replacement-lens biomaterial, polymethylmethacrylate (PMMA). Because the first prosthetic intraocular lens (IOL) was rigid, however, the incision required to insert it into the eye was large (encircling roughly half the cornea), required sutures, and made recovery long and outcomes variable.
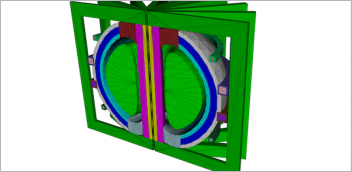
 Figure 2. Schematic of an inserter used for delivering an IOL through a corneal incision during cataract surgery. The IOL is loaded into the inserter, the door is closed, and the tip is snapped into place over the loading area. The doctor then inserts the tip into the incision and pushes the plunger, delivering the IOL into the eye. |
When deformable materials, such as hydrophobic acrylic and silicone, replaced PMMA in the early 1990s, incision size decreased dramatically because of the new materials’ ability to be rolled, folded and bent during insertion. As IOL materials evolved, the insertion process did, too, shifting from forceps to a tapering tube (similar to a syringe) that pushed the lens into the eye. Lenses are now being delivered through increasingly smaller incisions, ranging from 1.8 to 2.8mm.
With the size of the incision directly related to post-surgical aberrations in vision, engineers at Bausch + Lomb in Rochester, NY, continue to look for improvements. They have recently set an ambitious 1mm incision goal. To achieve this, ongoing research and development is focused on new lens materials, improved IOL geometry, and better inserter designs. That’s where finite element analysis (FEA), with its capability to realistically simulate a wide variety of physical phenomena, enters the picture.
Simulation Sees What Can’t be Measured
Engineers at Bausch + Lomb have been using Abaqus FEA, the Dassault Systèmes brand for realistic simulation, in biomedical applications for about 10 years. It was first employed to model the conformation and deformation of contact lenses on the cornea; this helped evaluate lens performance, including optical properties. Other applications have included improving cataract surgery tools and modeling manufacturing procedures.
“We use FEA in our iterative design process to shorten development time by analyzing each design or by developing design rules-of-thumb,” explains Robert Stupplebeen, design engineer and analyst at Bausch + Lomb.
In general, to create its FEA models, the Bausch + Lomb team first builds 3D CAD models in SolidWorks and then uses the software’s Associative Interface to import the model into Abaqus. From there, simulations are often coupled with other programs, such as SigFit, an optomechanical pre- and post-processor (developed by Abaqus Integration Program member Sigmadyne), and ZEMAX, a comprehensive optical design software package.
When starting a new product design project, “getting sufficient biological test data can be problematic,” says Stupplebeen. “With just about any biomedical product or process development, there are a lot of assumptions that need to be made.”
In the case of cataract surgery, the Bausch + Lomb product development team is focused on two primary modeling issues that can be confirmed by testing:
1. the insertion force required to implant the IOL, and
2. the geometry of the lens as it emerges from the inserter.
 Figure 3. Section view of the FEA model used to simulate lens (IOL) insertion during cataract surgery. The IOL (green) is being pushed by the plunger (purple) and is about to enter the inserter tip (blue), through which it is delivered into the eye. The lens, tip and plunger are modeled using deformable elements; the loading door (brown) and loading area (dark green) are modeled using rigid elements. |
But they also are interested in what can’t be measured in real life, such as the geometry and internal stresses of the lens when it’s in the inserter.
“We validate our model on the things we do know, and then utilize the rest of what the model tells us to gain a better understanding of the physical behavior,” says Stupplebeen. “Without FEA, all of these things are just unknowns.”
The cataract surgery simulation set-up requirements are stringent, says Stupplebeen: “The analysis is highly non-linear with large deformations, difficult self-contact, sliding contact, and hyper-elastic material properties. To handle all this in one model, we chose Abaqus/Explicit.”
The Model: Lens, Inserter, Incision
From an ophthalmologist’s point of view, the cataract surgical procedure is relatively simple: Take a standard IOL, which consists of a circular lens with four appendages (haptics) that stabilize the lens in the eye (see Figure 1); load the lens in the inserter and fill the inserter tube with a viscoelastic lubricant (see Figure 2); make a small corneal incision and remove the damaged crystalline lens using an ultrasonic device; then place the inserter in the incision and push the plunger, inserting the IOL. The surgery is outpatient and typically takes less than 10 minutes.
From an engineering perspective, however, the procedure is quite challenging, given the geometry: an industry-standard precision lens has a 6mm diameter, a center thickness of 1mm, and four haptics; an average incision is 2.8mm.
“It’s like trying to suck a Frisbee through a vacuum,” says Stupplebeen. “During the insertion, the lens can experience strains in excess of 60 percent.”
To simulate the lens insertion process, the Bausch + Lomb team modeled an acrylic lens, with average lens and inserter dimensions, and applied the following parameters to the model:
• hyper-elastic Neo Hooke material properties;
• Rayleigh damping to reduce low-frequency oscillations;
• general contact with zero friction (because of the smooth surfaces and lubricant);
• a non-linear pressure-overclosure relationship to reduce contact penetration; and
• mass scaling to reduce solve time by a factor of 10.
The loading area of the inserter was treated as rigid and modeled using R3D4 elements, while the lens, plunger and tip were all treated as deformable using C3D8R and C3D4 elements. The model of the lens and inserter, which are designed in tandem because of their close interrelatedness, is highly complex with approximately a quarter of a million elements with more than 100,000 increments. To run the five-hour analysis, the team used a Cray CX1 with Windows HP Server 2008.
|
Validating Lens Strain and Inserter Forces
By using Abaqus, the team was able to calculate the force applied on the inserter versus the displacement experienced by the lens, and then compare it with test data. The analysis yielded results that correlated well with the tests. The team was also able to measure strain on the lens while visualizing its deformation as it traveled through the inserter (see Figure 3). These peak strain measurements correlated well with extremely rare failure modes (tip fracture, lens tear and lens scratches), and were also found to occur in the same locations where past real-world failures had occurred (see Figure 4).
“Given the agreement between simulation results, physical tests and observations, the validated model is being used to reduce the likelihood of failure modes, reduce insertion force and develop the next generation of IOLs and inserters,” says Stupplebeen. “As surgeons strive for smaller incisions, we have to develop a more compressible material, thinner lenses and/or new inserter geometries.”
Clearly Visible FEA Benefits
Whatever the product development direction (and Bausch + Lomb is pursuing them all), Abaqus FEA is helping designers and engineers make predictions about what will and will not work. Because cataract surgery product design cycle time is typically about 18 months, with an additional 12 months for clinical trials, accelerating prototyping with realistic simulation provides tremendous bottom-line benefit.
“We recognize the significant return gained from continued investments in simulation,” says Stupplebeen. “Without a doubt, it has helped us shorten our time to market, decrease our development costs, and improve our product performance.”
Understanding Cataracts The natural lens in the eye (crystalline lens) lies behind the iris and the pupil, and is made up mostly of water and protein. The protein is arranged in a laminar structure that keeps the lens clear and lets light pass through it, focusing it on the retina. As we age, some of the protein may clump together, clouding a small area of the lens (a cataract). It has yet to be determined what causes the protein to cluster, but one recent finding suggests that fragmented versions of the protein bind with normal proteins, disrupting proper function. With aging, the eye’s lens slowly becomes thicker, less flexible and less transparent. Increasingly, larger areas of the lens become cloudy and opaque, and if left untreated (until the “overripe” stage), the cataract becomes white and can block vision completely. When vision becomes significantly impaired, it’s time to consider cataract surgery. Cataract surgery, the most frequently performed surgery in the U.S., has a high success rate. During the procedure, the ophthalmologist removes the clouded lens and, in most cases, replaces it with a clear plastic intraocular lens (IOL). New IOLs are continually being developed to further improve surgical outcomes for patients. To maintain healthy eyesight, get a baseline exam if you are over the age of 40, which is usually when early signs of disease and vision changes start to occur. Also, know your risk factors, such as family history, diabetes and smoking. To reduce cataract risk, eye-care practitioners recommend wearing sunglasses and wide-brimmed hats, which limit exposure to UV light. |
More Info:
Dassault Systèmes
Subscribe to our FREE magazine, FREE email newsletters or both!
Latest News
About the Author
DE’s editors contribute news and new product announcements to Digital Engineering.
Press releases may be sent to them via [email protected].